Mucosal Entry of HIV and Mucosal Immunity
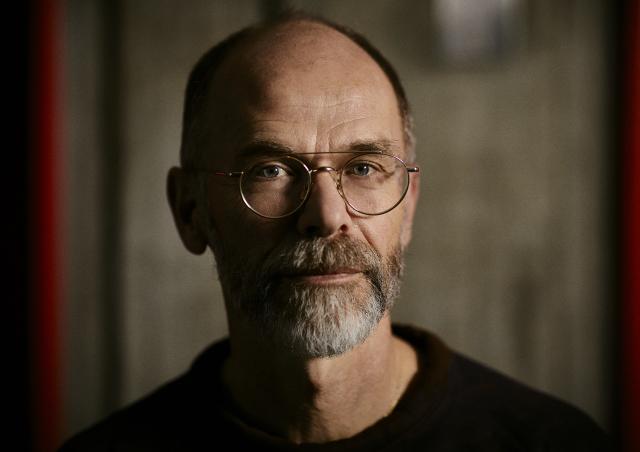
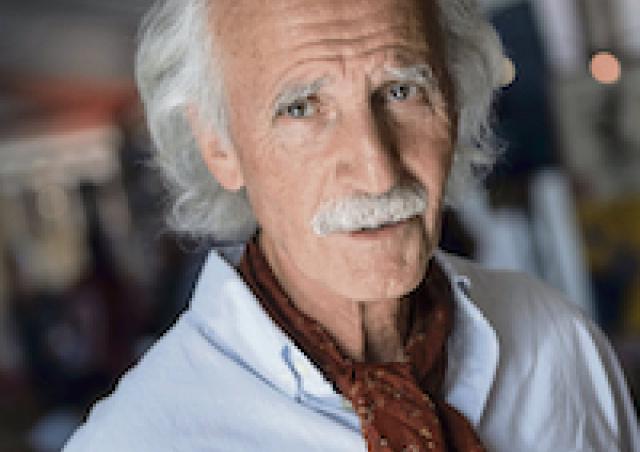
Leader(s)
HIV-1 is mainly transmitted mucosally during sexual intercourses, but the mechanisms of mucosal transmission, especially at the male genital tract, and protective mucosal genital immunity remain poorly understood. To elaborate anti-viral strategies against HIV-1 mucosal acquisition and persistence, our project addresses four main complementary topics.
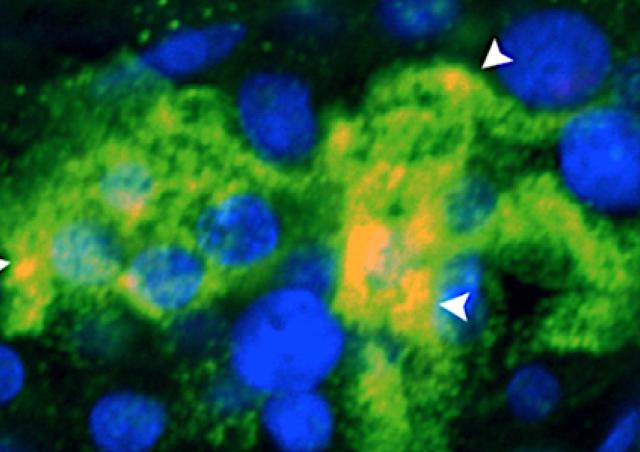
1. HIV-1 infection and persistence in the human adult male genital tract
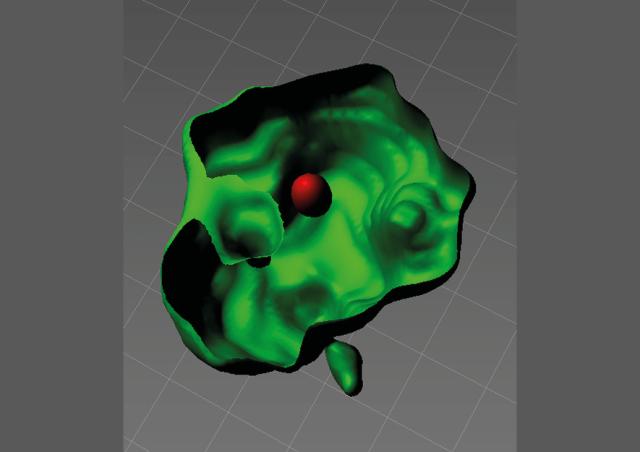
We have characterized how HIV-1 penetrates the male genital tract, and change the “only T-cell HIV-1 reservoir” paradigm by showing that tissue macrophages although form replication competent HIV-1 reservoirs. We are now identifying the mechanism of establishment and persistence of HIV at mucosal sites that preclude virus eradication.
2. HIV-1 in human platelets and impact on the patient immune response
We have shown that platelets from HIV-1+ patients under therapy nevertheless shelter infectious HIV-1 in correlation with sustained low CD4+T cell counts. We are now exploring the dynamic of this novel transient HIV carrier at the molecular level and its impact on HIV target cells to elaborate strategies for restoring proper CD4+ T cell counts in patients.
3. Neuro-immune control of mucosal HIV-1 transmission by neuropeptides: from the physiopathology to the characterization of a novel class of anti-HIV and HSV agents
All mucosa are innervated by peripheral neurons secreting neuropeptides locally, that we have recently shown to block mucosal HIV entry. We are now deciphering their antiviral roles in HIV-1 and HSV entry and potential use as preventive agent in vivo in an animal model.
4. Mucosal protection against HIV-1 by antibodies : from mechanisms to preventive HIV-1 strategies
To elaborate a mucosally active, prophylactic strategy, we will focus on highly exposed but seronegative individuals (ESN), uninfected despite unprotected sex with HIV+ partners, who develop mucosal antibodies with antiviral activities as sign of protection. We are now deciphering new mucosal IgA antiviral activities that are traditionally attributed to blood antibodies. The target on the virus recognized by these antibodies will be defined and used in novel anti-vrial strategies and for improving anti HIV vaccine design.
Together, these basic and translational studies should help design new prophylactic and therapeutic anti-HIV-1 and HSV strategies.