Project members
Projects
O-GlcNAcylation
A post-translational modification which depends on glucose availability.
O-GlcNAcylation is a reversible post-translational modification of cytosolic, nuclear and mitochondrial proteins. Like phosphorylations, O-GlcNAcylation can control their activity, their stability or their sub-cellular localization, but it uses a sugar (N-Acetyglucosamine or GlcNAc) rather than a phosphate to modify the serine and threonine residues of proteins. O-GlcNAcylation is closely dependent on the nutritional environment of the cell, and in particular on the availability of glucose. In fact, a fraction of the glucose which enters the cell is directed towards the hexosamine biosynthesis pathway and leads to the production of UDP-GlcNAc, the substrate used by OGT (O-GlcNAc Transferase) to O-GlcNAcylate the proteins. The reverse reaction is catalyzed by OGA (O-GlcNAcase), which removes the GlcNAc group from proteins. O-GlcNAcylation has been implicated in various chronic pathologies such as diabetes, obesity and cancer.
O-GlcNAcylation and Metabolic Diseases
Our previous work has shown that O-GlcNAcylation can participate in the phenomenon of gluco-lipotoxicity in hepatic and beta-pancreatic cells (Kuo et al., 2008; Guinez et al., 2011; Fardini et al., 2014; Filhoulaud et al., 2019), in particular by modifying the activity of transcription factors such as FoxO1 and ChREBP. While excess O-GlcNAcylation can have deleterious effects on certain diabetic complications (Issad et al., 2010), several studies suggest that O-GlcNAcylation also has protective effects on inflammatory processes and various cellular stresses (Baudoin and Issad, 2015). Using animal models with targeted OGT deletions, we are currently studying the role of O-GlcNAcylation in the macrophage and liver cell.
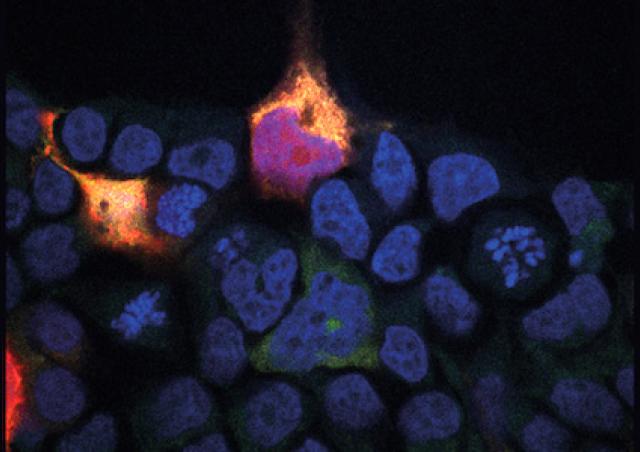
O-GlcNAcylation and cancer
Since glucose metabolism is strongly disturbed in cancers, we were also interested in the role of this modification in different cancer cell models (Kanwal et al., 2013, Groussaud et al., 2017, Jiménez-Castillo et al., 2022).
New tools to study O-GlcNAcylation
Our laboratory was part of the pioneering teams involved in the development of the BRET technique (Bioluminescence Resonance Energy Transfer) for the study of cell signaling. We are currently developing BRET tools to monitor, in real time, in living cells, O-GlcNAcylation in different cellular compartments: plasma membrane, cytosol, nucleus (Groussaud et al. 2017; Al-Mukh et al., 2020 ), and more recently, mitochondria (Pagesy et al., 2022).
O-GlcNAcylation in the macrophage
We have shown, in mouse macrophages and human monocyte-derived macrophages, that LPS stimulation induces a general increase in protein O-GlcNAcylation, suggesting an important role of this modification in TLR4 signaling (Al -Mukh et al., 2020). This increase in O-GlcNAcylation induced by LPS is due to a stimulation of the expression of GFAT2 (limiting enzyme of the hexosamine biosynthetic pathway), via the transcription factor FoxO1.
Moreover, we observed that O-GlcNAcylation has a protective effect against inflammatory processes in the macrophage. Indeed, in macrophages of mice invalidated for OGT, the absence of O-GlcNAcylation strongly increases the effect of LPS on the secretion of pro-inflammatory cytokines and on the induction of the enzyme NOS2 (Nitric Oxide Synthase 2). These results suggest that the LPS-induced increase in GFAT2 expression is a protective mechanism against excessive inflammation in macrophages. We are currently studying the mechanisms involved in this regulation and its potential role in inflammatory processes.
Our objective will be to determine, using ex vivo and in vivo approaches coupled with "multiomics" studies, the molecular and cellular mechanisms by which OGT negatively regulates pro-inflammatory processes and/or oxidative stress in the macrophage.
O-GlcNAcylation in liver cell
We have also developed a mouse model invalidated for OGT in the liver. This model revealed that O-GlcNAcylation plays a crucial role in the regulation of oxidative stress and hepatic homeostasis. Indeed, the decrease in O-GlcNAcylation in the liver cell is associated, from the age of 4 weeks, with an increase in the expression of markers of oxidative stress, pro-inflammatory cytokines, stress of the endoplasmic reticulum and DNA damage, and, at 8 weeks of age, the appearance of nodules of regeneration, fibrosis and blood markers of hepatic cytolysis (ALAT).
Interestingly, we have observed that these alterations can be fully prevented when the mice are weaned, at the age of 3 weeks, on a high-fat low carbohydrate diet (ketogenic diet) instead of the standard (high carbohydrate) laboratory chow diet. This suggests that OGT is necessary to cope with the increase in carbohydrate intake that normally occurs during the suckling-weaning transition in mice (Ortega-Prieto, Parlati, et al., 2023).
To investigate the consequences of hepatic OGT deletion in adult mice prior to the onset of severe liver injury, we also developed a mouse model of tamoxifen-inducible OGT deletion. Our objective will be to further characterize, using this animal model, the molecular mechanisms responsible for the hepatic alterations induced by the deletion of OGT in the hepatocyte, and to establish the potential of nutritional interventions as therapeutic strategies for management of liver diseases.
O-GlcNAcylation in mitochondria
Due to alternative splicing, 3 isoforms of OGT have been described: a long, nucleocytoplasmic form (ncOGT), a short form (sOGT) also localized in the cytosol and nucleus, and a form addressed to the mitochondria (mOGT). Two isoforms of OGA, long (L-OGA) and short (S-OGA), are also produced by alternative splicing. The long form of OGA, the most studied, is found mainly in the cytosol and in the nucleus. The short form S-OGA has remained very little studied to date. Our team recently discovered that the short OGA isoform (S-OGA) is specifically addressed to mitochondria, and that it controls the level of mitochondrial ROS (Pagesy et al., 2022, doi: 10.3390/cells11111827.).
Our objective will be to characterize, by bio-energetic, proteomic and BRET approaches, the targets of S-OGA in the mitochondria in order to elucidate its mechanism of action in the regulation of ROS production. We will also study its involvement in oxidative stress associated with metabolic diseases such as diabetes and obesity, and in particular in steatosis and steatohepatitis.