L'hepcidine est un peptide circulant clé qui maintient l'homéostasie systémique du fer dans l'organisme.
Les mutations affectant les régulateurs positifs de l'hepcidine ou le gène de l'hepcidine lui-même provoquent l'hémochromatose, une maladie génétique courante, caractérisée par une accumulation de fer. L'hepcidine est principalement produite par les hépatocytes et sécrétée dans le sang mais de nombreuses cellules et tissus expriment l'hormone dans des conditions pathologiques.
Au cours des dernières années, l'intérêt principal de notre groupe a été, sur la base des nouveaux modèles génétiques murins que nous avons générés, de définir les rôles physiopathologiques du facteur de transcription HIF-2 (Hypoxia Inducible Factor-2) et de l'hepcidine dans différents organes clés impliqués dans le maintien de l'homéostasie du fer corporel.
Notre équipe a mis en évidence le rôle de HIF-2 dans le métabolisme du fer en tant que régulateur essentiel de l'absorption du fer dans l'intestin et dans l'homéostasie systémique du fer (Peyssonnaux et al, JCI, 2007; Mastrogiannaki et al., JCI, 2009; Haematologica, 2012; Blood, 2012).
Plus récemment, nous avons cherché à définir les rôles locaux de l'hepcidine dans des conditions infectieuses/inflammatoires. En particulier, nous avons récemment démontré que, contrairement à l'hepcidine dérivée du foie qui agit comme une hormone endocrine (Zumerle et al. Blood, 2014), l'hepcidine peut être produite localement dans les épithélia, tels que la peau (Malerba et al., JCI, 2020) et l'intestin (Bessman et al., Science, 2020) pour contrôler la disponibilité locale du fer et les fonctions immunitaires.
Nos projets devraient apporter nouveaux paradigmes en recherche fondamentale et avoir des applications translationnelles dans de nombreux troubles inflammatoires tels que les maladies inflammatoires de l'intestin ou de la peau, qui se caractérisent par une homéostasie chroniquement dérégulée de l'épithélium ou encore dans le cancer dans lequel le contrôle de l'équilibre en fer est particulièrement crucial.
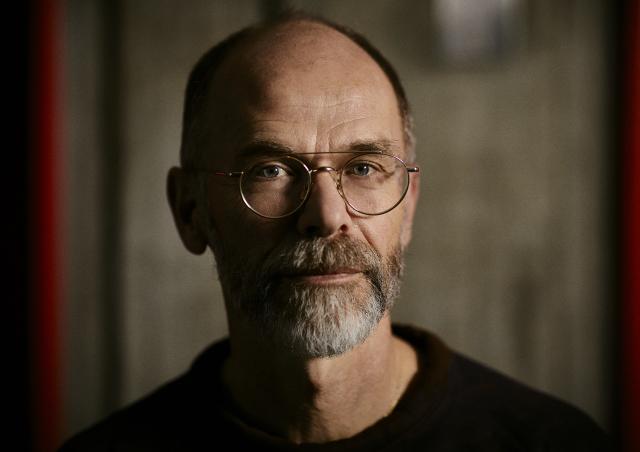
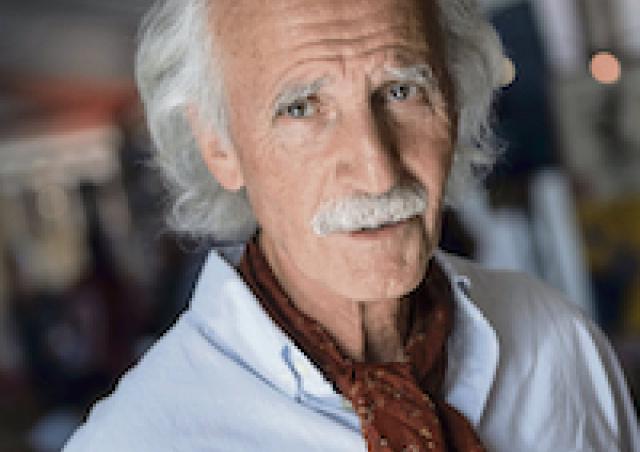
Les membres du projet
Project
Iron is an essential element critical for a multitude of biological processes at the cellular level (including catalyzing essential enzymatic reactions and electron transport) and at the systemic level for oxygen transport in hemoglobin. Both iron excess and iron scarcity have important consequences. Excess iron accumulation leads to the production of dangerous free radical species, responsible for epithelium injury and increasing the risk for cancer, while iron deficiency is one of the most frequently observed diseases in the world today, affecting as many as two billion people. Therefore, iron levels need to be tightly regulated in the organism. This regulation is ensured by hepcidin, a 25 amino acid circulating peptide hormone sought for many years, whose role in maintaining systemic iron homeostasis was discovered by members of the team in 2001.
Genetic studies in mice lacking or overexpressing hepcidin suggested that this peptide inhibits both iron absorption in the small intestine and the release of recycled iron from macrophages (Nicolas et al., PNAS, 2001; PNAS, 2002; Viatte et al., Blood, 2004; Blood, 2005). The established view is that plasma hepcidin inhibits iron efflux into plasma by directly binding to and thereby inducing the degradation of ferroportin (FPN), which is located on enterocytes and macrophages (Nemeth et al., Science, 2004). Hepcidin expression is upregulated by iron repletion, infection and inflammation and downregulated by iron deficiency, ineffective erythropoiesis and hypoxia (Nicolas et al. JCI, 2002) (see Figure 1) and can be targeted to treat iron overload disorders (Nicolas et al., Nat Genetics, 2003).

Mutations affecting hepcidin regulators or the hepcidin gene itself cause hemochromatosis, a common genetic disorder, characterized by excess iron overload of organs such as liver, heart, or pancreas. Accordingly, hepcidin knockout (KO) mice displayed iron overload (Lesbordes et al., Blood, 2006).
The discovery of hepcidin has brought a major contribution to the field of iron homeostasis. In the last two decades, hepcidin has been the focus of intense research, in order to clarify its role in iron homeostasis and in iron-related pathologies (Nemeth et al., Int J Mol Sci., 2021).
The majority of the studies on hepcidin focus on the liver, which is the major producer of the hormone. However, many cells and tissues express the hormone raising the possibility of hepcidin involvement at the single tissue level. In particular, we demonstrated for the first time hepcidin expression in myeloid cells infected in vitro and in vivo (Peyssonnaux et al., Blood, 2006). Concomitantly, a number of laboratories have shown that other tissues are able to synthesize hepcidin: heart, kidney, retina, brain, splenocyte, adipocytes, pancreas… The contribution of these tissues on circulating hepcidin and the specific function of hepcidin in these tissues were not known. In order to determine the role of these hepcidin-producing tissues, we have generated mice with floxed hamp1 alleles allowing tissue-specific gene deletion with the classical Cre-loxP strategy. Using this model, we demonstrated that hepcidin deletion specifically in the liver recapitulated characteristics of hemochromatosis, mimicking the iron overload phenotype of total hepcidin KO mice (Zumerle et al. Blood, 2014). More surprisingly, we found undetectable plasma hepcidin levels, indicating that cell types other than hepatocytes contribute in basal conditions negligibly to circulating hepcidin and suggesting novel, unanticipated roles, for locally produced hepcidin.
Originally identified as a cationic antimicrobial peptide (AMP) by its close structural similarity to the beta defensins, the expression and role of hepcidin in the intestine and skin, major sources of AMP production had never been investigated. We recently demonstrated that, in contrast to liver-derived hepcidin that acts as an endocrine hormone, hepcidin can be produced locally in these epithelia.

Axis 1. Role of skin hepcidin in infectious/inflammatory diseases
We showed that hepcidin is unexpectedly produced in the skin as a result of infection with Group A streptococcal infections (GAS), bacteria involved in the development of necrotizing fasciitis (Mariangela et al., JCI, 2020). Hepcidin produced by the epidermis of the skin is able to induce neutrophil recruitment at the site of infection by increasing the production of the neutrophil chemokine CXCL1 (Figure 2). In addition, unlike CXCL1, hepcidin is resistant to degradation by bacteria and could therefore be used as a drug to "force" the expression of CXCL1 and neutrophil recruitment. Indeed, the administration of hepcidin to mice helps their immune system to fight against infection and prevents bacterial invasion. Thus, hepcidin, by its ability to boost the immune system, could be considered as a therapeutic alternative in a large number of pathologies.
We are currently investigating the role of skin hepcidin in the context of psoriasis, a skin inflammatory disease with increasing incidence worldwide, for which new therapies are urgently needed.
Axis2. Role of gut hepcidin
Intestinal homeostasis depends on complex interactions between the intestinal epithelium, the host immune system, and the microbiota. Loss of this equilibrium may result in the development of inflammatory bowel diseases (IBD), which are represented by two main clinical forms, Crohn’s disease (CD) and ulcerative colitis (UC).
Role of DC-derived hepcidin
In a collaborative effort with the team of Greg Sonnenberg (Weill Cornell Medicine, USA), hepcidin was found to be produced by dendritic cells (DC) in the context of IBDs. DC-derived hepcidin controls local iron bio-availability to promote mucosal healing following tissue inflammation and damage (Bessman et al., Science, 2020) (Figure 3).
Role of IEC-derived hepcidin?
Hepcidin is produced by the intestinal epithelial cells (IECs). To probe the function of gut-derived hepcidin, we generated and validated mice with a specific ablation of hepcidin in intestinal epithelium.
Thanks to the generation of this new mouse model, we started to explore the role of gut hepcidin in physiological and inflammatory/infectious conditions.