Project members
Project
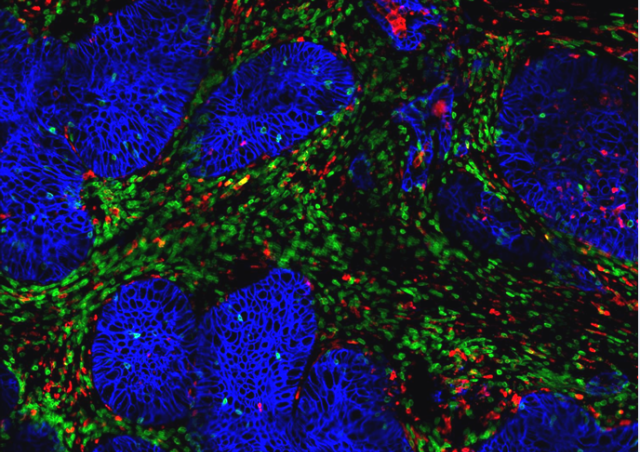
Immunotherapies trigger fruitful cooperation between T lymphocytes and myeloid cells in the microenvironment of regressing tumors.
Inspired by the work of surgeon W. Coley more than a century ago, we have developed mouse models in which it is possible to induce solid tumor melting, by mimicking a local infection to trigger an immune system reaction. We were thus able to observe frequent regressions and study the mechanisms involved, an original approach in view of the many works that have focused on the phenomena of tumor escape. Moreover, our readings convinced us that an effective immune response must have both an appropriate dynamic and spatial dimension to coordinate the action of different immune effectors (Bercovici and Trautmann, 2012).

It was in unexpected circumstances that we observed for the first time an activation of macrophages after immunotherapy: the tumor regression which followed the injection of a vaccine to specifically activate CD8+ T cells in mice, was preceded by an influx mass of myeloid cells. We were able to show that the latter are then activated by the IFNɣ produced by the CD8+ T cells and acquire cytotoxic activity against tumor cells (Thoreau et al., 2015). This was a first example of "ping-pong" between these two cell types.
We confirmed this observation in a second model, based on the use of a powerful inducer of type I interferons, IFNα and IFNβ: this time again, the regression is optimal in the simultaneous and local presence of the two immune effectors (Weiss et al., 2017).
The publication of our results challenged the dominant thought that macrophages were deleterious for anti-tumor immunity. But mentalities are changing, and it is now accepted that various treatments, including standard chemo- and radiotherapy treatments, anti-PD1/PDL1 and anti-CTLA4 immune checkpoint blockades, or adoptive transfers of TIL or CAR T, are are also accompanied by drastic remodeling of the myeloid compartment in responder patients, consistent with our predictions.
To go further, we tested the possibility of strengthening cooperation between T cells and macrophages to prevent tumor relapse, one of the main causes of cancer-related mortality. In particular, we considered that anti-PD1 treatments, which have revolutionized cancer treatment in recent years but do not yet allow all patients to be cured, could benefit from a combination with IFNα to activate more largely the interactions between immune cells that infiltrate tumor tissue. We have succeeded in our bet by showing that the local injection of IFNα near the tumour, combined with anti-PD1, induces complete regressions and prevents local relapses. Interestingly, it is the cooperation between CD8+ TILs and macrophages that is enhanced by this combined treatment, rather than the number or function of each of the effectors separately.
These results therefore provide important proof of concept: stimulated in an appropriate manner, and in this case only, the myeloid cells which abundantly infiltrate tumors can actively contribute, alongside T lymphocytes, to causing tumor regression. They are therefore not necessarily deleterious, contrary to the widely accepted idea over the past 20 years.
TGFβ blocks IFNα production and hampers the onset of tumor regression
Exploration of mice developing tumors spontaneously, however, suggested that these mice were much more difficult to treat than mice with transplanted tumors. Indeed, our first attempts at treatment with a STING agonist (DMXAA), revealed that the mouse model of spontaneous MMTV-PyMT tumors was resistant to the induction of tumor regression by this drug, unlike the transplanted model. derived from these same PyMT tumor cells. This observation, initially very disappointing, turned out to be of major importance. This finally allowed us to understand that MMTV-PyMT mice specifically resisted the induction of type I Interferon production, and that a key molecule in this inhibition was TGFβ. TGFβ accumulates in spontaneously growing MMTV-PyMT tumors, but not in transplanted PyMT tumors, highlighting the importance of the choice of mouse models used in pre-clinical studies (Guerin et al., 2020). We have also shown that macrophages that infiltrate tumors are the major source of IFNα produced after this type of therapeutic intervention. We were able to dissect a mechanism underlying signaling by the TGFβ receptor which, by involving the HDAC4 and IRF3 molecules, blocks the expression of type I interferons. This is how TGFβ, present in murine tumors spontaneous, blocks the anti-tumor action of molecules acting via the production of type I interferons.
By combining stimulation of the IFN type I pathway with an antibody blocking TGFβ, we were able to induce a regression of these spontaneous tumours. These results, published in Nature communications (Guerin et al., 2019), lead to an important notion: as several anti-cancer therapies involve the production of type I IFN to be effective, their combination with TGFβ inhibitors should potentiate the production of type I cytokines and therefore their effectiveness.
Thus, in a growing tumor where tissue repair phenomena involving TGFβ take place, the presence of the latter blocks the ability of macrophages to produce type I IFNs in response to danger signals. On the other hand, this lock lifted, macrophages become a major source of type I IFN, and induce many chemokines required to locally recruit immune cells.
In particular, we have shown that, by producing CXCL9, macrophages facilitate the recruitment of Th1 T cells, with a strong anti-tumor effect. Admittedly, macrophages do not recognize tumor antigens, but their joint activation with that of T lymphocytes would make it possible to eliminate even escape antigenic variants. In addition, IFNg produced by tumor antigen-specific T cells is essential to induce CXCL9 production and macrophage tumoricidal activity. The system is efficient because the exchange of information between T lymphocytes and macrophages is bi-directional.
If we consider the dynamics of the system, macrophages do not only intervene upstream, as the first line of defense of our organism, but can be considered as real assets for later events, when the adaptive system is mobilized.
We are currently focusing on clarifying the mechanisms of this cooperation between T lymphocytes and myeloid cells, macrophages and monocytes, at the different stages of tumor regression and we have addressed the repercussions on the establishment of a systemic and protective immunity against the occurrence of metastases.